Type 2 Diabetes — Causes, Symptoms, Treatment & Prevention
Type 2 Diabetes is the most common form of diabetes, developing when the body becomes resistant to insulin or when insulin production can’t keep up. This condition progresses gradually and is closely tied to lifestyle, genetics, and insulin resistance. Understanding it early supports prevention, timely diagnosis, and better long‑term health.
Compare with brain‑related insulin resistance here: Type 3 Diabetes (Alzheimer’s & Metabolism). External overview: CDC – Type 2 overview.

Causes and Risk Factors
The primary driver is insulin resistance: muscle, fat, and liver cells stop responding normally, so the pancreas produces more insulin to compensate. Over time, this demand fatigues beta cells and glucose rises.
- Family history and age (risk rises after 45)
- Abdominal obesity and physical inactivity
- Diets high in refined carbs and added sugars
- History of gestational diabetes
Ultra‑processed food patterns and sugary beverages accelerate risk. Early lifestyle changes can significantly lower the odds of developing this condition (NIH).
Signs and Symptoms
Warning signs can be subtle for years. Common clues include frequent urination and thirst, fatigue, blurred vision, slow‑healing wounds, and numbness or tingling in extremities. Because onset is gradual, screening is essential for those with multiple risks.
Insulin Resistance in T2D
In T2D, cells don’t use insulin efficiently; the pancreas works overtime until it can’t meet demand. As glucose rises, damage accumulates across the cardiovascular, kidney, nerve, and eye systems. Learn more in our guide to insulin resistance; clinical background: NIDDK.
Understanding Type 2 Diabetes
Type 2 Diabetes is the most common form of diabetes, affecting millions worldwide. It develops when the body becomes resistant to insulin or when the pancreas cannot produce enough insulin to keep blood glucose levels within a healthy range. This condition is closely linked to lifestyle factors, genetics, and insulin resistance.
Common Type 2 Diabetes symptoms include increased thirst, frequent urination, fatigue, blurred vision, and slow-healing wounds. However, many people may live for years without obvious symptoms, making regular screenings essential for early detection (CDC).
While genetics play a role, lifestyle changes can significantly reduce the risk of developing Type 2 Diabetes. Key strategies for Type 2 Diabetes prevention include maintaining a healthy weight, eating a balanced diet low in refined carbs and added sugars, engaging in regular physical activity, and managing stress. Learn more about dietary strategies in our guide to Intermittent Fasting & Diabetes.
Type 2 Diabetes treatment often involves a combination of lifestyle changes, blood sugar monitoring, and medications such as metformin. In some cases, people may also require insulin therapy. Research also shows that addressing insulin resistance through diet, exercise, and sleep improvements can help improve blood sugar control (NIH).

Type 2 FAQs
Can this condition go into remission?
Yes, remission is possible for some people, especially with significant weight loss, improved food quality, and regular physical activity. Clinicians often aim for sustained A1C improvement without glucose‑lowering meds for a defined period. Individual results vary and require medical guidance. See more practical strategies in our Intermittent Fasting guide and our Ultra‑Processed Food Detox resource.
Which eating patterns support better control?
Whole‑food forward patterns (Mediterranean, lower‑glycemic, high‑fiber, or carb‑conscious approaches) consistently improve insulin sensitivity. Some find time‑restricted eating helpful; coordination with a clinician is essential if you’re on medications. For meal ideas, explore Diabetes‑Friendly Easy Dinners.
What complications matter most long‑term?
Cardiovascular disease, chronic kidney disease, neuropathy, and retinopathy drive most morbidity. Early blood pressure, lipids, and glucose management, plus weight and sleep optimization, reduce risk. See clinical guidance at the American Diabetes Association.
Is it purely genetic?
Genetics influence risk, but environment and behavior strongly shape outcomes. Two people with similar genetics can diverge dramatically based on diet quality, activity, sleep, and stress. Lifestyle isn’t everything, but it is powerful.
When should someone be screened?
Adults with risk factors (e.g., higher BMI, family history, gestational history, hypertension, or dyslipidemia) should be screened periodically. Discuss timing with your clinician; earlier screening is prudent when multiple risks are present (CDC risk factors).
What role does sleep play in blood sugar control?
Sleep deprivation disrupts hormones such as cortisol, leptin, and ghrelin, which can increase appetite and reduce insulin sensitivity. Aiming for 7–9 hours of consistent, good‑quality sleep supports more stable glucose.
Are natural remedies effective for T2D?
Some supplements (e.g., cinnamon, berberine, bitter melon) have signals in research for improving insulin sensitivity. They can complement—not replace—clinician‑guided care. Always discuss with your healthcare team to avoid interactions.
How does stress affect this condition?
Stress raises cortisol and can elevate blood sugar. Simple daily practices—breath work, brief walks, stretching, sunlight exposure—help calm the nervous system and support metabolic health. See our Detox & Gut Health page for whole‑body strategies.
What’s the difference between T2D and prediabetes?
Prediabetes is a “yellow‑light” stage where glucose is elevated but not yet in the diabetes range. It’s a high‑leverage window for lifestyle change to prevent progression. Our insulin resistance guide explains why early action works.
How do A1C, fasting glucose, and CGMs fit together?
A1C estimates average glucose over ~3 months, fasting glucose captures a single morning reading, and continuous glucose monitors (CGMs) show real‑time trends. Used together, they provide a fuller picture for you and your clinician.
Diagnosis & Testing
Diagnosis typically relies on A1C, fasting plasma glucose, or an oral glucose tolerance test. Because the onset can be quiet, those with multiple risk factors should test periodically. Discuss your personal screening schedule with your provider; if numbers trend upward, earlier intervention generally yields better outcomes.
Treatment Options
Many start with lifestyle measures: nutrition upgrades, regular activity, weight management, stress reduction, and sleep hygiene. When needed, medications like metformin, GLP‑1 receptor agonists, SGLT2 inhibitors, and others may be added by your clinician to improve glucose, protect organs, and reduce cardiovascular risk. Medication choices are individualized based on goals, kidney function, side‑effect profiles, and cost considerations.
Lifestyle & Self‑Care
Daily choices compound. Small improvements—kept consistently—often beat large changes that are hard to maintain. Use the ideas below as a starting point, then build routines that fit your life.
Movement
- Weekly target: ~150 minutes of moderate activity (e.g., brisk walking, cycling, swimming) plus 2–3 days of strength training to enhance insulin sensitivity.
- Meal‑time walks: 10–15 minute walks after eating can blunt glucose spikes.
- Break up sitting: Stand, stretch, or stroll for 2–3 minutes every 30–60 minutes.
Nutrition Basics
- Center meals on non‑starchy vegetables, quality protein, and healthy fats.
- Choose fiber‑rich carbs (beans, lentils, quinoa, berries) and limit refined flour and added sugar.
- Consider time‑restricted eating with medical guidance if you use glucose‑lowering medications.
- Explore easy, practical meals: Diabetes‑Friendly Easy Dinners.
Hydration & Sleep
- Hydration: Drink water throughout the day; dehydration can nudge glucose higher.
- Sleep: Prioritize a wind‑down routine, cool dark room, and consistent sleep/wake times (7–9 hours).
Stress & Mental Health
- Short relaxation breaks (breathing, prayer/meditation, stretching) lower stress hormones.
- Social support helps—consider our community resources and local groups.
Monitoring & Tools
Meter checks, A1C labs, and sometimes CGMs help you see patterns. Pair numbers with notes about meals, movement, sleep, and stress so you can adjust the right lever. Technology supports awareness; your habits drive change.
Myths & Misconceptions
- Myth: Only overweight people get T2D.
Fact: People at any weight can develop this condition, though excess abdominal fat increases risk. - Myth: Cutting out all carbs cures diabetes.
Fact: Quality, quantity, and timing of carbs matter more than eliminating them entirely. - Myth: If you feel fine, you don’t need checks.
Fact: Many have minimal symptoms until complications appear; screening matters. - Myth: It’s purely genetic, so lifestyle doesn’t matter.
Fact: Genes load the gun; environment pulls the trigger. - Myth: Medications mean you’ve failed.
Fact: Meds are tools. They can protect organs while you improve lifestyle.
Prevention Checklist
- Keep a healthy waist circumference; track progress monthly.
- Build meals around whole foods; reduce ultra‑processed options (UPF detox guide).
- Move daily; add strength training 2–3 times weekly.
- Sleep 7–9 hours; keep a consistent schedule.
- Practice stress relief (breathing, prayer/meditation, nature time).
- Limit sugary drinks and refined carbs; hydrate with water.
- Schedule regular screening; discuss goals with your clinician.
When to Seek Medical Care
Call your clinician promptly for persistent high readings, symptoms of dehydration, chest pain, shortness of breath, sudden vision changes, or signs of infection. If you use insulin or glucose‑lowering medications, ask your care team for a personalized plan to prevent and treat low blood sugar.
Helpful Resources
- CDC: Type 2 overview
- NIH/NIDDK: Type 2 Diabetes
- ADA: Treatment & Care
- Insulin Resistance (LWWD)
- Intermittent Fasting & Diabetes (LWWD)
- Diabetes‑Friendly Easy Dinners (LWWD)
- Detox & Gut Health (LWWD)
- Type 3 Diabetes & Metabolism (LWWD)
Take the Next Step
If you or someone you love is at risk for Type 2 Diabetes, early action changes the story. Explore our guides, share this page, and join the Living Well With Diabetes community for practical tools, recipes, and support. Your daily choices are powerful—start small, stay consistent, and keep going.
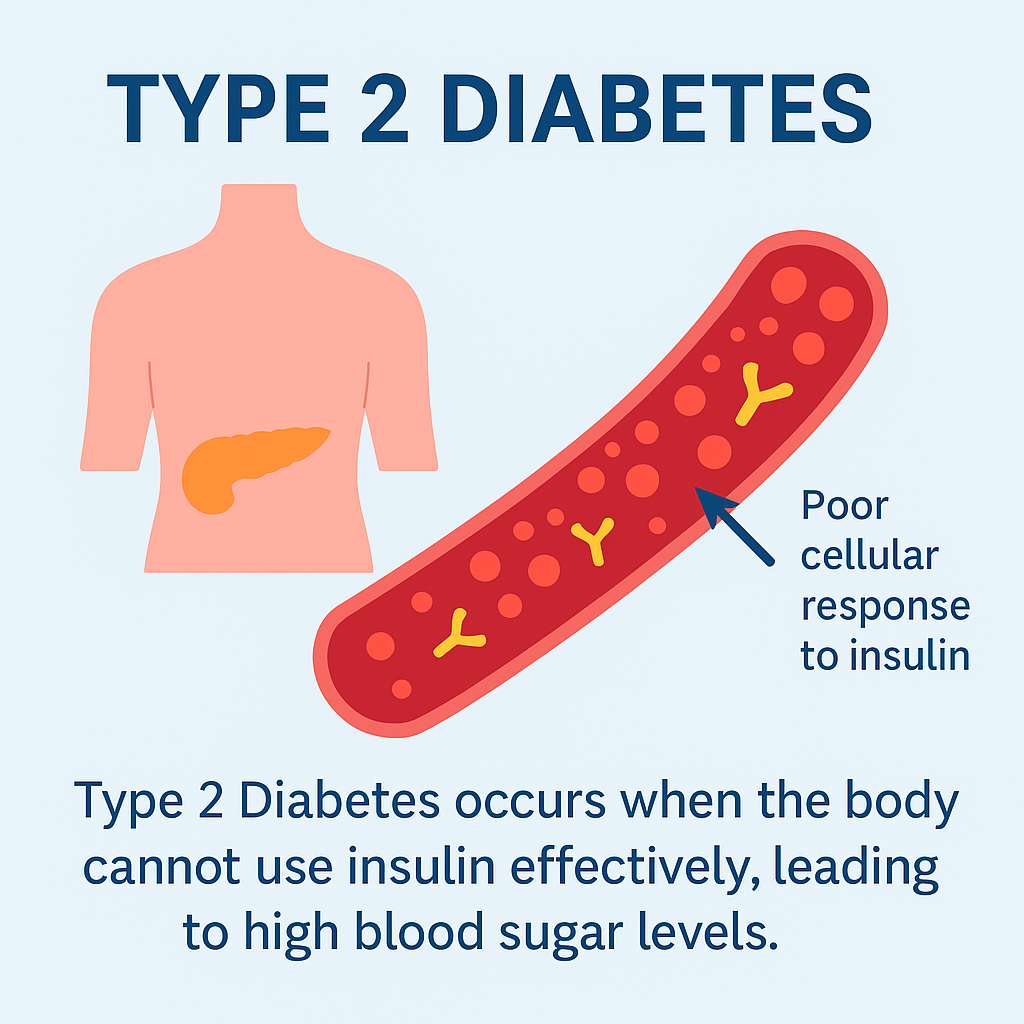
Table of Contents
Toggle